
Time for another revolution in medicines access The ‘test case’ of Herceptin
15/02/2013
The last fifty years is witness to a virtual explosion in the creation of new knowledge. Capitalism has used this characteristic of modern science and technology to constantly create products and tools to constantly revolutionize the productive forces. At the same time it is also seized with the necessity to control the expressions of new knowledge. Control over knowledge is one of the most important tool that modern day Capitalism uses to maintain its hegemony. Perhaps the most common expression of control over knowledge is the Intellectual Property system – which operates through the medium of patents, copyrights, trademarks, etc.
This dual nature of capitalism in the arena of knowledge creation – knowledge creation and its control are both embedded in the nature of capitalism. Without new knowledge and the creation of new products, capitalism is unable to survive. At the same time, it cannot allow the free use of such knowledge, as this jeopardizes the very basis of capitalist accumulation based on hegemony over the process of production. This inherent contradiction is starting to express itself in a new dilemma – control over knowledge production is now a fetter on creation of new knowledge.

TRIPS – a cruel agreement
This dilemma s being played out in the field of innovations that leads to discovery of new medical products. It is being played out in two very important ways. The 1980s and 1990s were a period of intense struggle, waged by developed capitalist countries, to put in place a global system that would legalise its hegemonistic control over knowledge. The result was the signing of the TRIPS (Trade Related Intellectual Property Rights) agreement in 2004. The TRIPS agreement legitimized the control over knowledge through a strengthened patent regime that was to be applicable to all countries in the world (with some limited waivers in the form of transition periods for developing and least developed countries).
The TRIPS agreement is a cruel agreement – what it basically says is that access to knowledge that can save lives would be limited to those who can pay (as individuals or through their governments). The decade of the 1990s saw the unfolding of one of the worst man-made tragedies ever, in the form of the HIV AIDS epidemic. Nominally, the disease is caused by a virus, but the conditions for the devastation it caused (and is still causing) was a human creation. In less than a decade after HIV infection was first detected in humans, the first drugs to effectively treat it were being rolled out. Yet it raged across the poorest countries of the world, especially in sub-Saharan Africa, decimating huge swathes of the population. Almost a whole generation succumbed to the disease in the region. Not because remedies were not available. Not because we did not understand how the spread of the disease could be stopped. But because these remedies were not allowed to reach those who needed them the most. They were not allowed to be used because a handful of CEOs of giant pharmaceutical companies priced these drugs way out of the reach of people who needed these drugs in poor countries. Sub-Saharan Africa was already reeling under massive debt burdens foisted on them by policies promoted by the IMF and World Bank. They were now asked to shell out money to buy drugs that would save their people – money that amounted to, in some cases, over 50% of the entire GDP of the country.
In 2001, and Indian company – Cipla – entered the fray. It announced that it would supply drugs to treat HIV AIDS at 1/40th (that is just 2.5%) of the price charged by multinational corporations. Drug prices of anti-retrovirals (those that treated HIV AIDS) fell from the earlier $12,000 per patient/per year to $300. Since then the prices of these early anti-retrovirals have fallen to less than $100 for a year’s treatment.
Biologics – the new frontier of disease control
The above story, known to many, merits repeating because it is now being played out in another area of medicinal products. The next new-frontier of disease control lies in finding remedies that can effectively cure and control cancers and several degenerative diseases. Cancers of different kinds are a cause for over 8 million deaths every year (i.e. almost 15% of all deaths) and 70% of these deaths occur in low and middle income countries. Even 3 decades back most cancers were considered a death sentence. No more so. Over the past decades new treatments and products are starting to win significant victories over a number of types of cancers. New products are being developed and many are already in use – many of which are a significant advance over existing treatments. As such opportunities open up, they are also opening up opportunities for pharmaceutical companies to reap super-profits at the expense of human misery. While the basic research for virtually all cancer treatments are done in public funded institutions, the ultimate products are controlled by a handful of companies.
Simultaneously we are seeing another development taking shape. Fewer and fewer new drugs that are significant advances over current treatments are being researched. Partly this is a consequence also of what we have noted earlier – the patents system, by controlling access to knowledge, finally also acts as a fetter to the creation of new knowledge. Most patents registered today do not protect an invention, they actually are designed to prevent others from doing research. Known as ‘patent thickets’ these patents prevent transmission of knowledge, and its further development. In India less than a handful of new medicines are introduced every year, yet several thousand patents are granted. This is a global phenomenon not restricted just to India. While the number of patents is growing, the number of new drugs that are being researched continue to fall alarmingly.
There is, however, and exception to this trend. The field of biotechnology is starting to live up to its earlier promise and is delivering entirely new forms of treatment. Thus while we have fewer drugs of promise that are being developed through the earlier route of chemical synthesis, exciting new treatment avenues are being opened up by research using the biotechnology route for drug development.
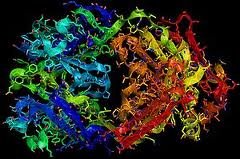
Drugs developed using biotechnology are different because they are produced in living cells. The molecules which make up these drugs are larger in size and more complex than the ‘small molecule’ drugs manufactured using the chemical synthesis method. The manufacturing systems used to produce these drugs need to be monitored differently. These drugs – termed as biologics – have several potential advantages. They can, theoretically, be tailored to hit specific ‘targets’ in the human body. This is of particular interest in diseases which are caused by altered or aberrant functioning of specific genes – such as in the case of several types of cancers. Traditional cancer drugs are called ‘cytotoxic’ drugs, i.e. they are poisonous to cells in the body. The basic principle on which they work is that they selectively kill cells that proliferate very fast (as happens in the case of cancer cells). However they are never entirely selective and that is why cytotoxic drugs have a range of side effects caused by the destruction or alteration of normal cells in the body as well. Biologics are being developed that only target specific gene sequences in cells and thus would have less side effects.
The Herceptin Story
One such drug that is a breakthrough drug is called trastuzumab. The drug is used to treat a certain kind of breast cancer that is particularly aggressive and difficult to treat or manage.
Trastuzumab works in a way that is very similar to the way antibodies work in the body. Antibodies are produced by the body’s immune system, which is the body’s defense system against foreign invaders – like viruses, bacteria, and other biological agents. They are able to recognise these foreign agents and bind to them. The body’s immune system then gets into action to destroy these foreign cells. Trastuzumab binds to a gene called the HER2 gene, that is more active in some breast cancer patients. The HER2 gene stimulates the growth of cancer cells. By binding to the HER2 gene, Trastuzumab suppresses its activity. It also stimulates the body’s own immune cells to destroy the tumour cells.
Trastuzumab belongs to a class of biologics that are called monoclonal antibodies. Monoclonal antibodies are produced from a single cell-line (hence the term ‘mono’), which is cloned to produce a very large number of cells. The cells are genetically engineered (i.e. a piece of foreign gene is introduced into the cell) to secrete the antibody we desire. Trastuzumab, for example, is made by substituting a portion of a human gene into a mouse using recombinant DNA technology. The mouse cells are thus ‘fooled’ into producing the antibody.
To continue the Trastuzumab story – the drug was marketed in 1998 by Genetech (later acquired by the Swiss multinational, Roche). It is sold under the brand name Herceptin. It is interesting to note that though the product has now been around for almost 15 years, Roche still enjoys global monopoly over the drug. The story would have been very different if Herceptin had been a drug that could be produced by the chemical synthesis route. Given the drug’s important public health benefit, many generic manufacturers (especially in India, the major centre of generic drug manufacture in the developing world) would be interested in producing their own versions of Trastuzumab. Herceptin was introduced in the global market at a time when the Indian Patent law allowed generic versions of patented drugs to be produced without any restrictions. The inability of Indian companies to come up with a generic version is related to special features that characterize biologics like Trastuzumab.
Unlike in the case of conventional ‘small molecule drugs’ it is never possible to produce an exact replica of the original drug. Biologics are extremely sensitive to the manufacturing process and the starting material. As the starting material is a living cell, it is impossible to have an exactly similar starting cell. Moreover very small changes in the manufacturing process can bring about changes in the final product. Thus, even in the case of the original product, there are variations in the product – between batches and even within the same batch. Thus the equivalents of generic versions of generics are called ‘biosimilars’.
Biosimilar manufacture is a relatively new area as the processes involved are entirely different from those used to produce drugs through the chemical synthesis route. Further, there are regulatory hurdles because the process of getting regulatory approval for biosimilars is more cumbersome than for ‘small molecule’ drugs. This is again because of the nature of biologics – because it is impossible to replicate the original drug, more data is demanded by regulatory agencies to prove that the quality, safety and efficacy profile of the biosimilar is identical to that of the reference drug (i.e. the original biologic). Consequently, in the case of biologics, patent barriers are not the only barrier to the production of biologics.
The time to act is ‘now’
Herceptin has recently been in the news because of two reasons. First, because of the interest being generated about use of Compulsory licenses (i.e. licenses issued to generic companies to manufacture patented drugs) after India issued its first compulsory license last year for another anti-cancer drug – sorafenib. The second reason is that it is only now that Indian companies have started acquiring the capacity and technical competence to produce biosimilars.
Because it now appears possible that biosimilars of Herceptin can be introduced, it is important to examine the economics and the public health importance of the drug. Treatment with Herceptin typically consists of 12 intravenous doses of the drug, administered every three to four weeks over the course of a year. Roche sells the drug for more than Rs.70,000 per dose. Clearly the cost is prohibitive for almost any Indian patient. The cost has to be seen in the context that breast cancer is the most prevalent form of cancer among urban women, and the second most prevalent for rural women According to the national cancer registry, over 1,00,000 women in India develop breast cancer every year (about 1 in 22 women in India stand at risk of getting breast cancer in their lifetime). Out of the total number of breast cancer patients, about 25% benefit from Herceptin (there are tests that can show which patients will benefit). Thus approximately 25-30,000 women would benefit from the use of Herceptin. Importantly, Herceptin is useful in the most aggressive form of the cancer, which typically afflicts younger patients. Yet because of the misuse of the monopoly situation that Roche enjoys, barely 5% of eligible patients are able to access the drug, and many of those who do are put on a lower dosage than recommended.
The situation cries for an immediate remedy. There are several issues that need to be addressed in order to expedite the entry of biosimilars of Herceptin in the Indian market. First, patent barriers need to be removed by expeditious issue of a compulsory license. The patent status of Herceptin is not clear in India as it is the subject of several litigations, however a compulsory license is the fastest way to make sure that patents are not a barrier to introduction of biosimilars. Simultaneously regulatory procedures need to be streamlined to ensure that entry of biosimilars are fast-tracked, while of course ensuring that quality is not compromised. Finally, public investment is necessary to build larger capacity in India to produce biosimilars.
Herceptin is a test case. If the attempt to get Inidan biosimilars of Herceptin in the market is successful, it has the potential to open the doors for a range of other biosimilars of other new biologic drugs that are already in the market or are being developed. Cipla’s pioneering action in 2001 revolutionized HIV AIDS treatment. Biosimilars produced by Indian companies can change the face of treatments for many diseases, now considered virtually untreatable, not just in India but across the world. There is no reason why the experience of a 97.5% drop in prices, seen in the case of HIV AIDS drugs when generics were introduced, cannot be replicated in the case of biosimilars. A bold and responsive government and regulatory agencies need to act in tandem to make this a reality. The time to act is now.