Know Your Covid-19 Variants from Scariants
08/01/2023
The media’s focus on the SARS-CoV-2 variant spreading in China may prove excessive. Far more concerning variants are spreading rapidly in the United States and Europe.
The news of China opening up from Covid-19 protocols and its current epidemic has overtaken the threat from two emerging SARS-CoV-2 lineages—XBB and BQ.1. In China, the BF.7 variant is spreading, which is much closer to the original Omicron strain of the virus that causes the Covid-19 disease. Our immunity gained from vaccines or infections should, therefore, continue to protect us from infections partially and more against serious illness.
The threat from the Chinese variant, as the media calls it, is much lower than from the variants in the United States and Europe. It has nothing to do with the geography of the virus: it is simply the genetic distance of the XBB and BQ.1 sub-variants from what our bodies have experienced, either as vaccines or previous infections. Eric Topol, founder-director and professor of molecular medicine at the Scripps Research Institute, has talked about variants of the SARS-CoV-2 virus we need to worry about and the “scariants”. Scariants are the variants used to create fear and frighten us, but they are just another strain, hundreds of which exist at any given time. In the Topol nomenclature, the XBB and BQ.1 strains are variants to worry about, while the BF.7 emerging in China may only be a scariant!
I am not getting into how the virus strains are named. The question here is not which one descended from where but how different these sub-variants are from the original Omicron strain. While BF.7, the dominant sub-variant in China, is not that distant from the original Omicron variant, the BQ.1 and XBB sub-variants are quite distant. It also matters which part of the virus mutates. If the mutations are in the spike protein region, they may improve the ability of the virus to infect us. Again, the BQ.1 and XBB sub-variants have significant changes in the spike protein, meaning they have an improved ability to bypass our immunity in the initial stages of infection.
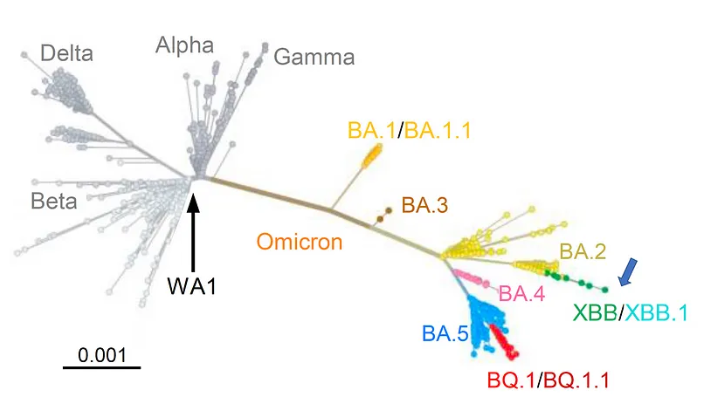
Figure 1: Phylogenic tree from Cell, Wang et al.
Why should this matter to us? Eric Topol discusses the three properties we must note in any new variant. Is it more virulent? Does it cause more deaths? Or is it more infectious, that is, it transmits more easily from person to person? Or is it more immune evasive, meaning that even if we have been vaccinated or infected, our body’s immune system does not recognise the virus, which means we can get re-infected? Initially, the success of the “new” virus lineages was due to their greater transmissibility or the ease with which they could infect people. With the population already infected or having received multiple vaccine doses, the success of the current variants would depend on how effectively they can evade our immune system. If they are more effective at immune escape than other variants, the new strains will become variants of concern among the hundreds of new sub-variants that continuously emerge.
The BQ and XBB sub-variants of SARS-CoV-2 Omicron are rapidly expanding in North America and Europe. The journal Cell has reported a study, “Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants”, by Wang et al. It concludes that “…the neutralisation of BQ.1, BQ.1.1, XBB, and XBB.1 by sera from vaccinees (vaccinated persons: author) and infected persons was markedly impaired”. The Cell paper continues, “Monoclonal antibodies capable of neutralising the original Omicron variant were again largely inactive against these new subvariants…Together, our findings indicate that BQ and XBB subvariants present serious threats to current COVID-19 vaccines, render inactive all authorised antibodies, and may have gained dominance in the population because of their advantage in evading antibodies.”
Why, then, so much noise about the Chinese BF.7, which does not appear to have the immune escape properties of BQ.1 and XBB subvariants? Even in India, we are focussing more on incoming passengers from China, as Europe and the United States are doing, but what are the preparations for the new subvariants? The XBB.1.5 strain has emerged in the last two weeks as the dominant strain in the United States and is likely to take over globally.
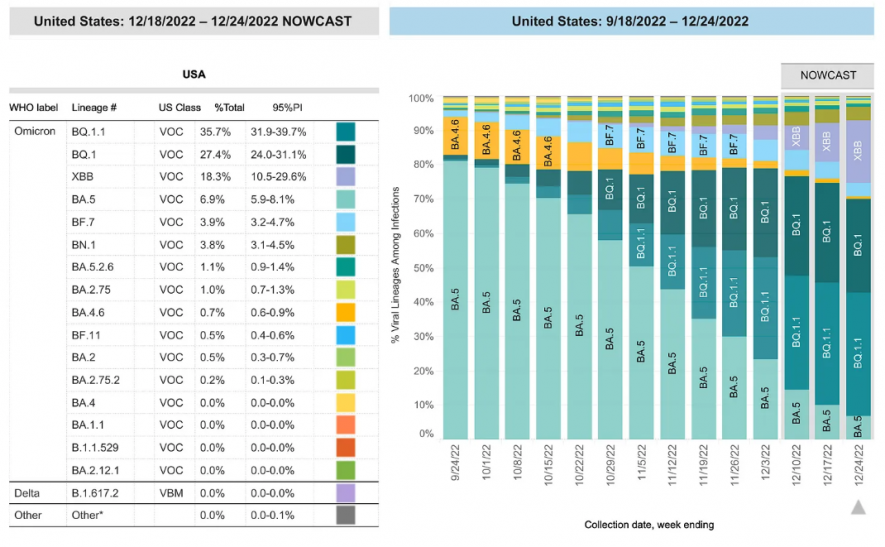
Figure 2: https://covid.cdc.gov/covid-data-tracker/#variant-proportions
The reason for fearing passengers from China and asking for Covid-19 tests is that after having relaxed its zero-Covid policies, cases are exploding in China. That is why there is the need to test if Chinese passengers are Covid-free before they start their journey from China and re-test them after disembarking. While China has condemned these measures as discriminatory, they are as much political as epidemiological. At this point, the XBB-1.5 has led to sharp increases in hospital admissions in North East United States (the New York-Boston area) and will likely emerge as the dominant global strain. The BF.7 strain emerging in China is close to other Omicron strains that have already caused major spikes in India and elsewhere.
Before China relaxed the restrictions of its zero-Covid policy, the western media was campaigning about how this disastrous policy was wrecking China’s economy. Now that it has been relaxed, the same media are going to town on how disastrous it is that China is lifting its Covid-19 restrictions. Damned if it does, and damned if it doesn’t!
China’s zero-Covid policy, particularly when the virus was completely new and during the Delta version, saved millions of lives. When the United States had 11 lakh deaths, and India 5.3 lakh, China had a minuscule about 5,000 deaths. A detailed article published on 1 January by Tings Chack in MR Online explains why China pursued its zero-Covid policy. When the pandemic began, China, with a population five times the United States, had a tenth of the ICU beds of the United States. China strengthened its public health infrastructure for three years before lifting the zero-Covid protocols. All accept it needed to lift those restrictions: whether it should have been done the way it was is a question to leave for historians.
The Chinese government has changed Covid-19 from a Class A to B disease, which means reporting will be once a month. But as infection numbers rise quickly, a lack of official numbers will fuel speculation of China hiding data because it is bad and hundreds of thousands are dying. In the major urban centres in China, the numbers have risen steeply over the last 30 days, but social media reports of hospital collapses and mortuaries overflowing do not seem on the scale we saw initially in Wuhan or the rest of the world during the Delta spikes. It will be much more helpful if China releases the official numbers. Of course, in the huge spikes we now witness, testing infrastructure is tremendously challenged to carry out millions of daily tests. But this is one part of China’s infrastructure that should weather this storm better, as China had been testing millions every day earlier.
I expect a total number of those infected, including those who recover, in the tens, if not hundreds of millions, before the current wave subsides. Consider the figures China has supplied to the WHO. The WHO site reports that in the two days from 3 January to 5, there have been 10.5 million confirmed Covid-19 cases and 32,679 deaths. But the peak appears to be receding in many major urban areas. Let us not forget China is a massive country and home to a fifth of the world’s population.
The test for China is not the number of Covid-19 infections but the number of the seriously ill—those admitted to hospital—and the dead. It still confronts two challenges: First, handling the severe cases in urban areas that peak after two or three weeks, and second, addressing the inevitable rise of infections in rural areas after the urban peaks. As written before on these pages, large numbers of deaths occur when the health infrastructure collapses, overwhelmed by massive numbers of serious cases. The unavailability of ICU beds and oxygen shortages led to high death rates in India and other parts of the world during the Delta peak in late 2020. This is the test China must pass. Though it has increased ICU beds 2.4-fold in the last three years, the high number of infections can still overwhelm them, particularly in rural areas.
Everywhere, the Omicron spikes produced high infection numbers. Though deaths per 1,00,000 were much lower than in the Delta variant, the much higher number of infections meant that, in absolute terms, there was also a high number of deaths, particularly among the unvaccinated. In China, contrary to western media campaigns, most people have been vaccinated with two doses, and the booster doses number 2.3 times the population, higher than in countries like the United States, with a 1.8-time coverage. Given that not all the vulnerable—older populations and the immune-compromised—have received booster doses, China needs to target this section, particularly with its new adenovirus vector nasal vaccine. (India, China, Iran and Russia are the only countries administering vaccines from the nasal route.)
We need to ask whether the raging Omicron infections in China will produce new and more dangerous variants. There is no evidence it has. The genome sequences China is submitting to the global GISAIDs and testing of passengers from flights from China show the BF.7 sub-variant is still the dominant strain in China. This variant is genetically much closer to the Omicron virus that swept the world earlier, and our immunity from vaccines and previous infections should provide immunity against this strain. Though the Indian government has issued warnings against BF.7, the danger—given air traffic between the United States, the United Kingdom and India—is from XBB.1.5, the rapidly emerging dominant strain in the United States. As we know, where the United States leads, the United Kingdom and European Union surely follow!
India’s adenovirus vector nasal vaccine should be foregrounded in our Covid-19 preparedness, not so much for the BF.7 strain but the XBB.1.5 strain. Though much better equipped with knowledge of how to treat Covid-19 and its various manifestations today, India’s challenge is implementing this knowledge, particularly if and when a new wave appears. The Covid-19 pandemic is by no means over, and new challenges will likely emerge in 2023, including the unsolved long Covid, apart from the higher-than-usual deaths post-pandemic.